
Given the newest wave of transparency with breast augmentation procedures, there has been a surge in people talking about the “plane” of the implant placement. As medical topics like this are often dispersed into the culture, patients and potential patients are confused about the nomenclature and making inaccurate conclusions about what the words mean.
As a plastic surgeon who has performed countless breast implant surgeries, I want to walk you through the different implant placement options and how each one affects your results, recovery, and long-term satisfaction. Hopefully, this can help to clarify some of the confusion out there.
Why Implant Placement Matters
The position of a breast implant—whether it's placed above or below the muscle, or somewhere in between—affects the final look, feel, and behavior of the breast. It influences how natural the breast appears, how well the implant is supported over time, and how it may interact with your lifestyle, including physical activity and aging.
Let’s break down the four main placement techniques: submuscular, dual-plane, subfascial, and subglandular.
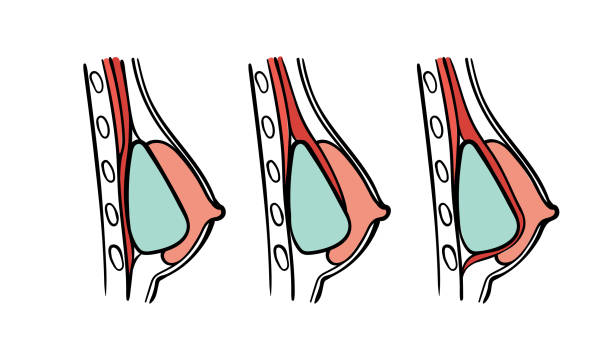
Subfascial Dual-Plane Submuscular
1. Submuscular Placement
(Complete Submuscular or Total Submuscular)
In this method, the implant is placed completely beneath the muscle. This means that either the pectoralis major muscle is elevated, the implant is placed under, and the muscle is closed back over the implant, or another nearby muscle (serratus) is elevated to match up with the pectoralis muscle to provide complete muscle coverage of the implant. Although this was once a standard approach for breast augmentations and breast cancer reconstructions, the limitations of this approach have largely led to it being abandoned for other techniques. However, this term and technique often create confusion with submuscular vs dual-plane (discussed later) because in modern times, when surgeons use the term “under the muscle” they usually are referring to a dual-plane approach rather than a traditional total submuscular approach.
| Pros: | Cons: |
|
|
Best For: Lean individuals with minimal natural breast tissue who need the muscle to provide additional coverage or patients who have had problems with recurrent capsular contracture.
2. Dual-Plane Placement
The dual-plane technique is a hybrid approach that places the upper part of the implant beneath the muscle, while the lower part rests under the breast gland. To achieve this, the surgeon partially release the lower attachments of the pectoralis major muscle, allowing the implant to "slide" into a more natural teardrop shape. This is the technique that is most commonly referred to as “under the muscle.”
| Pros: | Cons: |
|
|
Best For: Patients seeking a natural look who want to cover the edges of the implant, and for patients who are very thin with minimal natural glandular tissue and need additional implant coverage.
3. Subfascial Placement
This is a technique that, while not new, has been getting more coverage recently in the media and in plastic surgery circles. In this technique, the implant is placed under the fascia—a thin but strong layer of connective tissue that covers the pectoralis muscle—but above the muscle itself. Many surgeons, such as I, have been performing “over the muscle” implant placement with this technique for years.
| Pros: | Cons: |
|
|
Best For: Patients who want a more visible implant look without the downsides of muscle distortion or in patients who have their own glandular/soft tissue coverage.
4. Subglandular Placement
In this approach, the implant sits directly beneath the breast tissue and above the muscle (and fascia). This was more common in the early years of augmentation but still has a role in modern practice in some patients although the benefits of subfascial augmentation have replaced “true” subglandular placement for some surgeons.
| Pros: | Cons: |
|
|
Best For: Patients with adequate breast tissue who want a very quick recovery and a more visible implant edge, and a rounder look.
How I Help You Decide
As a surgeon, I evaluate many factors before recommending the ideal placement method: your body type, lifestyle, breast tissue quality, goals, and whether this is a primary or revision procedure.
There’s no one-size-fits-all answer, and what’s right for one patient might not be right for another. My job is to personalize the approach to your anatomy and goals, using the latest techniques and safest practices to give you a beautiful, long-lasting result.
Final Thoughts
Implant placement is one of the most critical decisions in your breast augmentation journey. Understanding the differences between submuscular, dual-plane, subfascial, and subglandular positioning can empower you to ask the right questions and feel confident in your surgical plan.
If you’re considering breast augmentation or have questions about implant position, I’d be honored to guide you through the process with expertise, honesty, and artistry.
Ready to take the next step? Schedule a consultation and let’s explore what’s best for you.


